In an ICU, every minute counts. If a ventilated patient’s oxygen levels start dropping, doctors need to know quickly whether changing a ventilator setting or giving a drug will help or hurt.
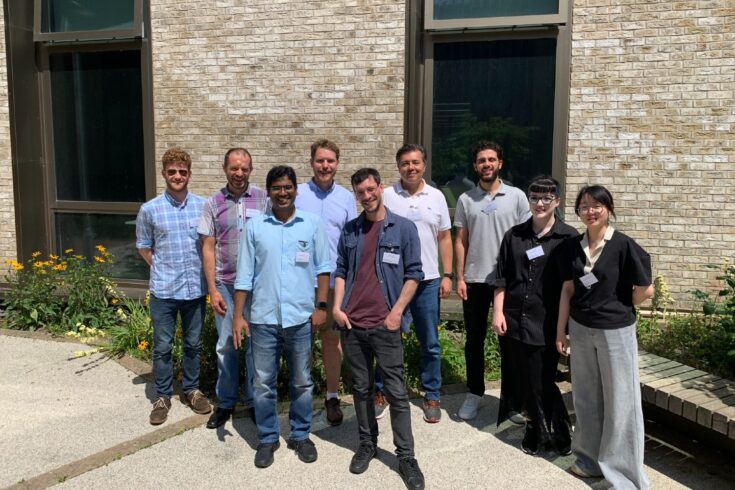
Our work at the CHIMERA (Collaborative Healthcare Innovation through Mathematics, EngineeRing and AI) helps medical professionals more effectively interpret, monitor, and project physiological changes in critical care situations.
About CHIMERA
CHIMERA is a hub for mathematics and medicine based at UCL. It’s supported by the Engineering and Physical Sciences Research Council.
Our mission is to leverage the university’s collaborative strengths to unlock new value from complex and underused ICU data, transforming it into clinically meaningful insights. In doing so, we aim to highlight the need for more streamlined data collection processes and closer collaboration between clinicians and scientists.
CHIMERA brings together engineers, mathematicians, statisticians, clinicians, and computer scientists to collaborate on challenges spanning deep learning, biophysical modelling, and mathematical modelling. By iterating between clinical needs and technical innovation, we create mathematical and computational models that are grounded in both biology and real-world practice.
With access to anonymised data from over 40,000 ICU patients across University College London Hospital and Great Ormond Street Hospital, we are building data-driven tools that help clinicians better understand, monitor, and predict physiological changes in critical illness.
Building dynamic virtual twins for ICU care
We are two PhD students on CHIMERA.
Developing biophysical models
One of us (Manuel) has developed biophysical models grounded in physiology, physics, and mathematics that provide a dynamic representation of human physiology. This framework offers a structured yet adaptable model that, once fine-tuned with individual patient data, can mirror personal physiological states.
These ‘virtual twins’ simulate how the human body behaves and responds during illness and recovery and can give us a clearer view of what is happening inside the body, when this is challenging (or even impossible) to observe directly.
Using real-world ICU data
The other of us (Jun) has been supporting the digital twin work by using real-world ICU data collected over time, applied retrospectively to continuously update patient-specific digital twins. The process of adjusting unknown parameters in the model to match observed data, known as dynamic calibration, helps keep the models aligned with data as it changes over time.
Adapting in real time to patient data
Many existing models are built once and remain fixed, making them less suitable for capturing the fast-moving changes ICU patients often experience. In contrast, our digital twins with dynamic calibration tools are designed to adapt in real time as patient data evolves.
While we are still some way from deploying in clinical settings, our methods have already been retrospectively demonstrated as successful in a few case studies, showing that the output of models after dynamic calibration can capture the trend of the observed data.
Providing an extra set of eyes to the clinicians
At the heart of our work is a simple goal: to help clinicians make better, more informed (and ideally faster) decisions.
Our virtual twins could help here. By incorporating patient data into our models, we create a ‘What‐if?’ sandbox. What if we increase the pressure on the ventilator? What if we reduce sedation? The model provides a sneak peek of how the patient might respond. Then, because of our dynamic calibration methods, the picture can stay up-to-date as new data comes in.
This is not about replacing doctors, it is about giving them extra insight. When a clinician sees a prediction that a patient’s lungs will respond poorly if they change a parameter, they can choose to pause and reconsider the available options.
Building the future framework for critical care
CHIMERA is laying the foundation for a new paradigm in critical care, one where computational models are both clinically relevant and rapidly deployable. The framework we are developing is not confined to a single condition, patient group, or hospital.
By building tools that are modular, adaptable, and rooted in fundamental physiology, we are creating methods that can be applied across diverse healthcare settings. Examples of these include managing sepsis in an adult ICU or supporting cardio-respiratory physiotherapy by modelling the amount and efficiency of secretion removal maneuvers in patients.
By bringing clinicians, engineers, and scientists together from the start, CHIMERA built better bridges between research and practice. This close collaboration has allowed us to develop the work quicker and with better interdisciplinary grounding.
With all the learned lessons we are now in the position to develop a fully integrated system that will allow data to be collected and processed in real time which will help us validate the models further.