Published in the journal Biomaterials, this represents an important step forward in being able to carry out medical research without the use of animals.
This crucial research was funded by the Biotechnology and Biological Sciences Research Council (BBSRC) and the Engineering and Physical Sciences Research Council.
Novel bioengineering
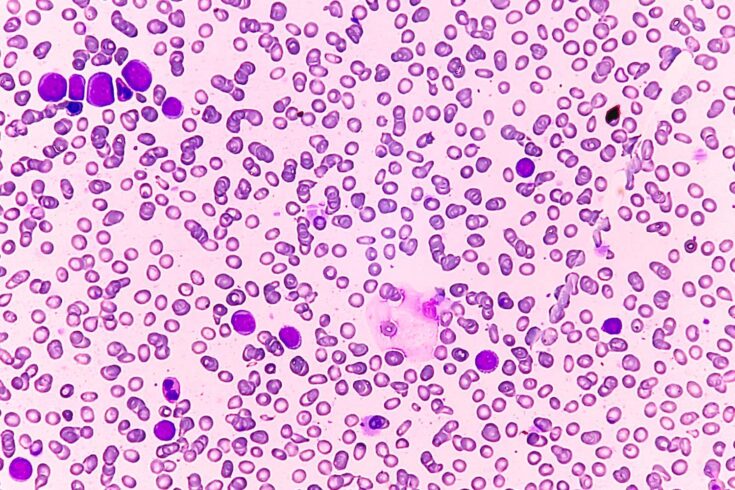
The study details the efficacy of chimeric antigen receptor (CAR) T-cell therapy, a promising new blood cancer treatment, in targeting acute myeloid leukaemia (AML), the most common leukaemia in adults.
This novel bioengineered model successfully delivered the kind of human-relevant insights and information that current research methods, which rely on animal models, have so far been unable to achieve.
Animal models
Leukaemia cancers are caused by mutations in hematopoietic stem cells (HSCs), which then rely on interactions with the bone marrow for their growth and survival.
However, studying these stem cells outside of the body is particularly challenging.
Once removed from the bone marrow, HSCs quickly change or die, making them challenging, or impossible, to work with in laboratories.
Until now, research teams have had to rely on animal models to test new drugs that could target blood cancers.
CAR T-cell therapy
Now, a team led by scientists at the University of Glasgow has been able to successfully carry out research on leukaemic HSCs.
They achieved this by inserting them into bioengineered jelly-like substances, called hydrogels, that mimic the natural bone marrow environment.
The team targeted the cancer cells with CAR T-cell therapy to find out if it could effectively target the disease.
While this is an early-stage study, the approach opens the door to more accurate pre-clinical testing.
Over the next decade, it could help improve the development of safer and more effective therapies.
Acute myeloid leukaemia
While CAR T-cell therapy has shown promise for other blood cancers, its application to AML has been hindered by a number of issues, including toxicity to local healthy cells.
Combining CRISPR-Cas9 gene editing with CAR T-cell therapy might have the potential for selectively targeting AML cells while sparing healthy tissue, by making healthy cells ‘invisible’ to CAR T-cells.
However, validating the effectiveness of this combination of treatments before clinical trial has been complicated by the differences between humans and animal models.
Crucial new insights
Using their bioengineered stem cell model, the team were able to provide key new information on the efficacy and safety of CAR T-cell therapy for AML.
They found that conventional testing methods, typically cells in a Petri dish, both overestimated the effectiveness of CAR T-cell therapy and failed to predict its harmful effects on healthy cells.
The new findings have clear implications, not only for future research on CAR T-cell therapy for AML, but also on approaches to pre-clinical CAR T-cell testing.
Improving patient outcomes
Dr Hannah Donnelly, one of the lead authors of the study and a research fellow at the University of Glasgow said:
There is a major translational gap in cell therapy development.
Conventional, over-simplified testing methods often fail to predict how therapies will behave in humans.
This gap leads to high failure rates in clinical trials, driving up costs and delaying treatments for patients.
By using human cells combined with hydrogels to mimic the complex structure of the bone marrow in the lab, we’ve shown that it’s possible to assess both the effectiveness of therapies and detect off-target effects much earlier, well before they reach the expensive clinical trial stage.
Our results highlight the potential of non-animal technologies for studying and developing new leukaemia therapies.
This approach could reduce reliance on animal models in drug testing over time, ultimately paving the way for more efficient and effective development of therapies for patients.
Delivering real-world impact
Professor Anne Ferguson-Smith, BBSRC Executive Chair, said:
This approach not only accelerates progress towards safer, more effective treatments for acute myeloid leukaemia, but also reflects UKRI’s commitment to supporting cutting-edge research that delivers real-world impact.